It starts the same way every time — you're awake, you're moving, but nothing lands.
You wake up after four or five hours of sleep. You go through the motions at work, but you're not sharp—and you know it. Your manager's noticed. In the evening, you scroll instead of doing anything that used to matter to you. Those coding projects, the cyber security courses you're paying for, the bike gathering dust—you look at them and feel nothing. No pull toward them. No spark.
You call it "just existing and hanging on."
And here's what makes it worse: you've been in therapy. You've been doing the work. Your therapist even showed you the numbers—your depression score dropped by half. From 19 to 9 on the PHQ-9. That's supposed to be significant progress.
So why does it still feel like you're stuck?
Your Score Dropped 50%—So Why Do You Feel the Same?
A 50% reduction in your depression score isn't a small thing. Clinically, that meets the threshold for a genuine treatment response. Your therapist was pleased because the data says something real happened.
But when you look at your life—at the hobbies you've abandoned, the subscriptions you're not using, the activities that used to excite you now triggering only exhaustion—the number doesn't match the experience.
Here's what most people don't realize: that disconnect isn't a sign that the therapy failed. It's actually what you'd expect to see at this stage.
The One Symptom That Always Heals Last
Depression isn't one thing. It's a collection of symptoms—disturbed sleep, concentration problems, feelings of worthlessness, fatigue, and more. And these symptoms don't all respond to treatment at the same rate.
Some improve relatively quickly. Others are notoriously stubborn.
That feeling you described—having "no pull" toward things you used to enjoy—has a clinical name. It's called anhedonia. And research consistently shows that anhedonia is the last symptom to improve.
One study examining depression treatment found that the extent of anhedonia repair was notably less marked than overall depression improvement across multiple treatments. It lags behind. This isn't unique to you. It's the pattern.
Your other symptoms improved enough to cut your score in half. The pleasure and motivation piece is moving more slowly—but that's how recovery actually works.
You're not failing to recover. You're recovering in the order recovery happens.
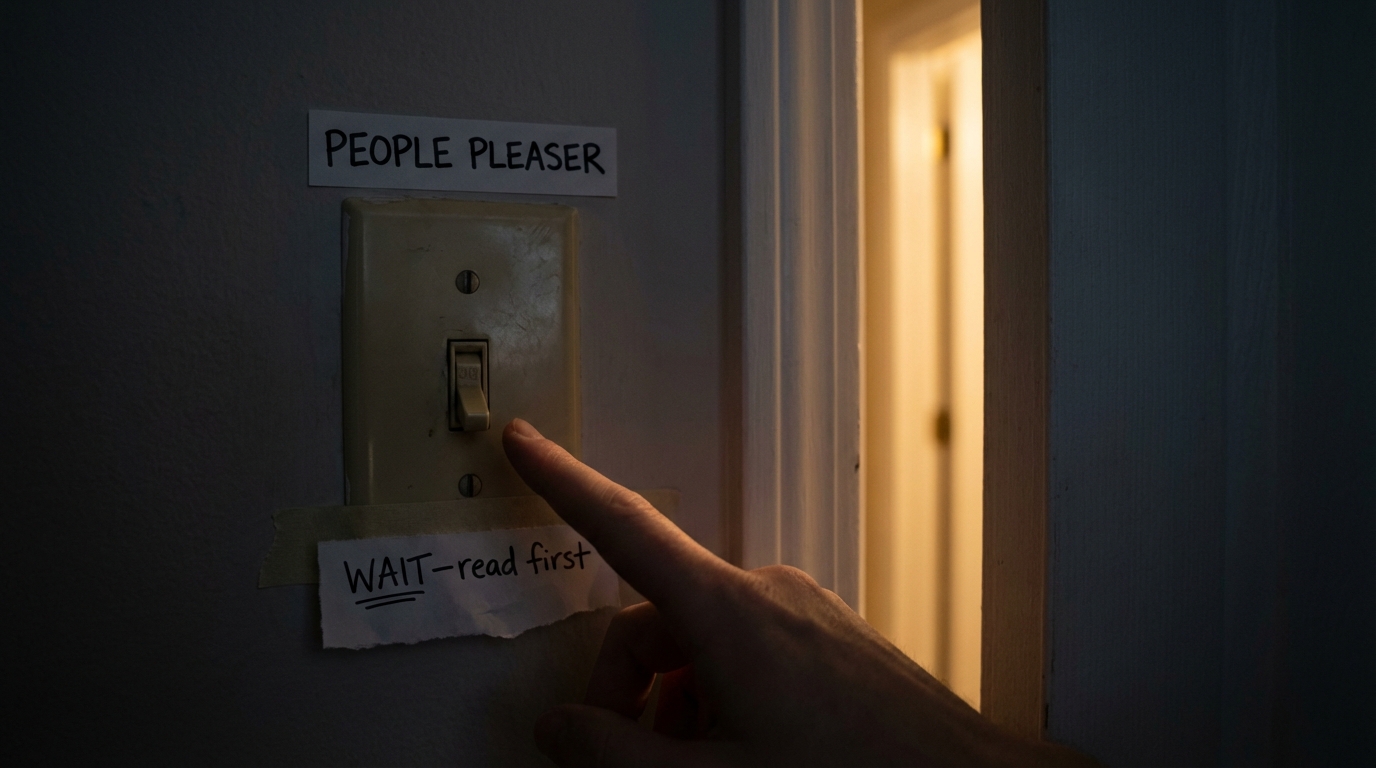
The Waiting Trap That Keeps You Stuck
Now let's look at what you've been doing while waiting to feel better.
You're not doing your hobbies because there's no motivation. No spark. You figure you'll start again when you feel better—when the pull returns.
This seems logical. The sequence in your mind is:
- 1. Feel motivated
- 2. Then take action
- 3. Then feel good
But with depression, that sequence is broken. And waiting for step one is waiting for a signal that isn't coming.
Why 'Wait Until You Feel Like It' Has It Backwards
Here's what the research shows—and it might sound counterintuitive:
With depression, action has to come first. The motivation follows the action, not the other way around.
This isn't just theory. A meta-analysis of 16 studies with 780 participants found that simply scheduling and doing activities—regardless of motivation—had a large effect on depression. The effect size was 0.87, which is substantial.
Even more striking: this approach is as effective as cognitive therapy and antidepressant medication. Not as a supplement. As a standalone treatment.
You don't need insight. You don't need to understand your childhood. You don't need to change your thought patterns first. You schedule, you do, and the brain starts to recalibrate.
The motivation comes after.
The Proof Is Already in Your Life
Think about when you reconnected with that old colleague. You went to their house, went out into town. How did that feel?
It was actually nice. You said so yourself.
But here's the question: did you feel motivated to go before you went?
Not really. You just kind of made yourself do it.
And there it is. Action first, feeling followed.
The same thing happened when you took your mother out shopping. You did it, and something good came from it. These weren't flukes. They were experiments you ran without knowing it.
The results are in. The reversed sequence works.
The Sleep-Depression Loop Nobody Explains
There's another piece here—your sleep. Going to bed at 4 AM, getting up at 8 or 9. That fear of falling asleep, connected to losing something or letting go.
You might think of poor sleep as just another symptom of depression. Something to endure while you work on the "real" problem.
But sleep and depression don't work that way. They form a bidirectional loop.
Your depression disrupts your sleep—yes. But your disrupted sleep also maintains your depression. Research shows this relationship runs both directions. Each condition worsens the other.
This means sleep isn't just a consequence to wait out. It's a lever. Improving it creates momentum against the depression, not just results from depression improving.
Your therapy review noted sleep showed the least improvement—which means it's also where there's the most room to make gains.
Why 'Just Go to Bed Earlier' Misses the Point
You've tried going to bed earlier. It doesn't work. You lie there and the resistance gets worse.
That's because "just go to bed earlier" ignores the fear entirely. You mentioned a fear of falling asleep—something about losing control or letting go.
This isn't irrational. Fear of falling asleep connected to losing control is actually a recognized pattern. For some people it develops after loss or trauma—the experience of things slipping away without consent. Sleep requires surrender, and if surrender feels dangerous, your nervous system fights it.
The good news: this specific kind of sleep problem has specific approaches that work. It's different from general sleep hygiene advice. Your therapist approved additional sessions partly to work on this directly.
Putting the Pieces Together
Let's put the pieces together.
Your PHQ-9 dropped 50%. That's documented progress meeting clinical criteria for treatment response.
The anhedonia—the "no pull" toward activities—is lagging because anhedonia always lags. You're not stuck. You're in the part of recovery that feels most like being stuck. There's a difference.
Waiting to feel motivated before acting is waiting for a broken signal. The sequence with depression is reversed: action first, feeling follows. You've already proven this works with the colleague visit and taking your mother out.
Your sleep isn't just a symptom to endure—it's part of a bidirectional loop that you can interrupt. The fear piece needs direct attention, not just willpower.
One Action for This Week
Pick one small activity. Not a triathlon. Something small—a 15-minute walk, or 15 minutes of one of those cyber security courses you've been ignoring.
Schedule it. Write down when you'll do it.
Then do it without checking if you feel like it first. Don't ask yourself if you're motivated. That question is a trap right now. Just do the thing.
Notice what happens. Not whether you felt like doing it beforehand—notice what happens after.
This is the practice. One small action, scheduled, completed without the motivation check.
The Reframe That Changes Everything
"In the part of recovery that feels most like being stuck."
That's where you are. Not stuck. Not failing. In a specific phase that has a specific character—and it's not permanent.
The therapy is working. The anhedonia is moving slowly because that's what anhedonia does. And you have something you can do right now that doesn't require waiting to feel better first.
What's Next: You mentioned a mental to-do list of about twenty items weighing on you, and your wife noticing you're speaking slower than usual. There's something important to understand about how cognitive load and processing speed work during depression—and why a long mental list creates paralysis rather than action. Understanding this changes how you approach the demands on you without adding more burden to an already-strained system.





Comments
Leave a Comment